Physical and Medical Standards
Appendix A
Guidelines with regard to physical and medical standards given in notification of AFCAT 01/2026 for candidates are as follows:-
- In this section, standardized guidelines for the physical assessment of candidates for commissioning through AFCAT into flying and ground duty branches in the IAF are elaborated. The purpose of these guidelines is to lay down uniform physical standards and to ensure that the candidates are free of health conditions that may hamper or limit their performance in the respective branch. The guidelines enumerated in this section are meant to be applied in conjunction with the standard methods of clinical examination.
- All candidates during their induction should meet the basic physical fitness standards which will enable them to proficiently undergo the training and the subsequent service in varied climatic and work environments. A candidate will not be assessed physically fit unless the complete examination shows that he/ she is physically and mentally capable of withstanding the severe physical and mental strain for prolonged periods. The requirements of medical fitness are essentially the same for all branches, except for aircrew in whom the parameters for visual acuity, anthropometry and certain other physical standards are more stringent.
- The medical standards spelt out pertain to initial entry medical standards. Continuation of medical fitness during training will be assessed during the periodic medical examinations held at NDA/ AFA prior to commissioning. They are not exhaustive, in view of the vast spectrum of diseases. These standards are subject to change with the advancement in the scientific knowledge and change in working conditions of Armed Forces.
- Laboratory and Radiological
Investigations for Special Medical Board
- Hematology: Complete Haemogram (Haemoglobin estimation, Total Leucocyte Count with Differential Leucocyte Count, Platelet Count).
- Hb Electrophoresis will be carried out in candidates for commissioning to exclude Haemoglobinopathies.
- Biochemistry: Liver function test (LFT), Renal Function Test (RFT), Blood glucose estimation (Fasting and two hours after 75 g anhydrous glucose/82.5 g glucose monohydrate loading), Lipid profile.
- Urine Routine Examination (RE) and Microscopic Examination (ME)
- ECG
- Radiology:
- Radiograph Chest PA view in all candidates.
- Radiograph Lumbosacral Spine: AP and Lateral views in all candidates.
- In addition to the above radiographs, Cervical Spine - AP and Lateral views, Dorsal Spine - AP and Lateral views will be carried out in all candidates being assessed for flying duties.
- USG Abdomen and Pelvis.
- Any other additional investigation deemed necessary will be conducted during the Appeal stage.
- Every candidate, to be fit for the Air Force, must conform to the minimum standards laid down in the succeeding paragraphs. The physical parameters should fall within the acceptable ranges and should be proportionate.
- The residual effects of old fractures/ injuries are
to be assessed for any functional limitation. If there is no
effect on function, the candidate can be assessed fit.
Following categories should be meticulously assessed:
- Spine Injuries. Cases of old fractures of spine are unfit. Any residual deformity of spine or compression of a vertebra will be cause for rejection.
- Nerve Injuries. Injuries involving the trunks of the larger nerves, resulting in loss of function, or neuroma formation, which causes pain significant tingling, indicate unsuitability for employment in flying duties.
- Keloids. The presence of large or multiple keloids will be a cause for rejection.
- Surgical Scars. Minor well-healed scars for e.g. as resulting from any superficial surgery do not, per se, indicate unsuitability for employment. Extensive scarring of a limb or torso that may cause functional limitation or unsightly appearance should be considered unfit
- Birth Marks. Abnormal pigmentation in the form of hypo or hyper- pigmentation is not acceptable. Localized, congenital mole/ naevus, however, is acceptable provided its size is < 10 cm. Congenital multiple naevi or vascular tumours that interfere with function or are exposed to constant irritation are not acceptable.
- Subcutaneous Swellings. Lipoma will be considered fit unless the lipoma is causing significant disfigurement/ functional impairment due to the size/ location. Neurofibroma, if single will be considered fit. Multiple neurofibromas associated with significant Café-au-lait spots (more than 1.5 cm size or more than one in number) will be considered unfit.
- Cervical Rib. Cervical rib without any neuro-vascular compromise will be accepted. Meticulous clinical examination to rule out neuro-vascular compromise should be performed in such cases. This should be documented in the Medical Board proceedings.
- Cranio-facial Deformities. Asymmetry of the face and head or uncorrected deformities of skull, face or mandible which will interfere with proper fitting of oxygen mask, helmet or military headgear will be considered unfit. Major deformities even after corrective surgery will be considered unfit.
- History relating to Operations. A candidate who has undergone an abdominal operation involving extensive surgical intervention or partial/ total excision of any organ is, as a rule, unfit for service. Operation involving the cranial vault with any residual bony defect will be unfit. Major thoracic operations will make the candidate unfit.
- Chest Shape and Circumference. The chest should be well proportioned and well developed. Any chest deformity likely to interfere with physical exertion during training and performance of military duties or adversely impact military bearing or are associated with any cardio-pulmonary or musculoskeletal anomaly are to be considered unfit. Minimum acceptable chest circumference in male candidates for commissioning is 77 cm. The chest expansion must be at least 05 cm for all categories of candidates. For the purpose of documentation, any decimal fraction lower than 0.5 cm will be ignored, 0.5 cm will be recorded as such and 0.6 cm and above will be recorded as 01 cm.
- Height
- Ground Duty Branches. The minimum height for entry
into ground duty branches is as follows:-
- Male – 157cm.
- Female - 152 cm.
Note 2:- Candidates of North East and Hilly states ethnicity includes Gorkhas, Kumaonis, Garhwalis, Assamese and those belonging to the states of Nagaland, Manipur, Mizoram, Meghalaya, Arunachal Pradesh, Tripura, Sikkim and hilly areas of Uttarakhand. - Flying Duty Branches. The minimum height (both male
and female) for entry into flying duty branches is as
follows:-
- Pilots, Flight Test Engineers (FTE) and WSO of Su 30 MKI - 162 cm.
- Officers and airmen who apply for aircrew duties, other than F(P), FTE duties and WSO of Su-30 MKI - 157 cm.
- Ground Duty Branches. The minimum height for entry
into ground duty branches is as follows:-
- Sitting Height, Leg Length and Thigh
LengthAcceptable measurements of leg length, thigh length
and sitting height for such aircrew will be as under:-
a) Sitting height: Minimum- 81.5 cm Maximum- 96.0 cm b) Leg Length: Minimum- 99.0 cm Maximum- 120.0 cm c) Thigh Length: - Maximum- 64.0 cm - Body Weight Parameters The acceptable weight range for candidates is given at Appendix A (Male candidates) and Appendix B (Female candidates) to this chapter Candidates outside the given weight range for their age and height will not be acceptable.
- Pulse. Persistent sinus tachycardia (> 100 bpm) as well as persistent sinus bradycardia (< 60 bpm) are unfit. In case bradycardia is considered to be physiological, the candidate can be declared fit after evaluation by Medical specialist/cardiologist.
- Blood Pressure. An individual with systolic blood pressure greater than or equal to 140 mmHg and/or diastolic blood pressure greater than or equal to 90 mmHg shall be rejected.
- Cardiac Murmurs. Evidence of organic cardiovascular disease will be cause for rejection. Diastolic murmurs are invariably organic. Short systolic murmurs of ejection systolic nature and not associated with thrill and which diminish on standing, especially if associated with a normal ECG and chest radiograph, are most often functional.
- ECG. Any ECG abnormality detected at SMB/Recruitment Medical Examination will be a ground for rejection. Benign ECG abnormalities like incomplete RBBB, T wave inversion in inferior leads, T inversion in V1 to V3 (persistent juvenile pattern), LVH by voltage criteria (due to thin chest wall) may exist without any structural heart disease. Echocardiography should be performed in all such cases to rule out an underlying structural heart disease and opinion of Senior Advisor (Medicine)/Cardiologist should be obtained.
- Congenital Cardiac Anomalies. All congenital cardiac anomalies will be declared unfit.
- Cardiac surgery and interventions. Candidates with history of cardiac surgery/ intervention in the past will be considered unfit. Respiratory System
- Pulmonary Tuberculosis. Any residual scarring in pulmonary parenchyma or pleura, as evidenced by a demonstrable opacity on chest radiogram will be a ground for rejection. Old treated cases with no significant residual abnormality can be accepted if the diagnosis and treatment was completed more than two years earlier.
- Pleurisy with Effusion. Any evidence of pleural thickening will be a cause for rejection. At the time of appeal, these cases will be subjected to detailed evaluation with appropriate investigations by Pulmonologist/Medical Specialist.
- Bronchitis. History of repeated attacks of cough/wheezing/bronchitis may be manifestations of chronic bronchitis or other chronic pathology of the respiratory tract. Such cases will be assessed unfit and will be subjected to detailed evaluation with appropriate investigations at the time of appeal by Pulmonologist/Medical Specialist.
- Bronchial Asthma. History of repeated attacks of bronchial asthma/wheezing/ allergic rhinitis will be a cause for rejection.
- Radiographs of the Chest. Definite radiological evidence of disease of the lungs, mediastinum and pleurae are criteria for declaring the candidate unfit.
- Thoracic surgery. Candidate with history of any major surgery of the thorax will be considered unfit. Gastrointestinal System
- Head to toe examination. Presence of any sign of liver cell failure (e.g. loss of hair, parotidomegaly, spider naevi, gynaecomastia, testicular atrophy, flapping tremors etc) and any evidence of malabsorption (pallor, nail and skin changes, angular cheilitis, pedal edema) will entail rejection.
- Gastro-Duodenal Disabilities. Any past surgical procedure involving partial or total loss of an organ (other than vestigial organs/gall bladder) will entail rejection.
- Diseases of the Liver. If past history of jaundice is noted or any abnormality of the liver function is suspected, full investigation is required for assessment. Candidates suffering from viral hepatitis or any other form of jaundice will be rejected. Such candidates can be declared fit after a minimum period of 6 months has elapsed provided there is full clinical recovery; HBV and HCV status are both negative and liver functions are within normal limits. History of recurrent jaundice and hyperbilirubinemia of any nature is unfit.
- Disease of the Spleen. Candidates who have undergone partial/ total splenectomy are unfit, irrespective of the cause for operation.
- Anterior abdominal wall EPID including
femoral hernia.
- Fit
- After 24 weeks of surgery (open as well as laparoscopic) provided there is no recurrence or post-op complications
- Unfit
- All current or operated cases of incisional hernia
- All cases of current anterior abdominal wall hernia.
- Fit
- After 01 year of hernia repair surgery (open as well as laparoscopic) provided there is no recurrence or post-op complications
- Unfit
- All cases of current inguinal hernia.
- Fit
- Abdominal Surgery A candidate with well-healed scar post conventional abdominal surgery (except appendicectomy through right iliac fossa incision, refer par 3.5.9 (b)) will be considered fit after 24 weeks provided there is no potential for any recurrence of the underlying pathology, no evidence of incisional hernia and the condition of the abdominal wall musculature is good.
- Anorectal Conditions. The examiner
should do a digital rectal examination and rule out
haemorrhoids, sentinel piles, anal skin tags, fissures,
sinuses, fistulae, prolapsed rectal mass or polyps.
- Fit
- After rectal surgery for polyps, haemorrhoids,
fissure, fistula, ulcer or pilonidal sinus, provided
there is no residual/recurrent disease.
- Anal Fissure, Hemorrhoids: After 12 weeks of surgery.
- Pilonidal Sinus: After 12 weeks of surgery.
- After rectal surgery for polyps, haemorrhoids,
fissure, fistula, ulcer or pilonidal sinus, provided
there is no residual/recurrent disease.
- Unfit
- Rectal prolapse even after surgical correction.
- Active anal fissure/External Skin tags.
- Hemorrhoids (external or internal).
- Anal Fistula
- Anal or rectal polyp
- Anal stricture
- Faecal incontinence
- Fit
- Ultrasonography of Abdomen
Liver- Fit
- Normal echo-anatomy of the liver, CBD, IHBR, portal and hepatic veins with liver span not exceeding 15 cm in the mid- clavicular line.
- Solitary simple cyst (thin wall, anechoic) upto 2.5 cm diameter provided that the LFT is normal and hydatid serology is negative.
- Hepatic calcifications to be considered fit if solitary and less than 01 cm with no evidence of active disease like tuberculosis, sarcoidosis, hydatid disease or liver abscess based on relevant clinical examinations and appropriate investigations.
- Unfit
- Hepatomegaly more than 15 cm in mid-clavicular line.
- Fatty liver –
- Grade 1 Fatty liver with abnormal LFT.
- Grade 2 and 3 Fatty Liver.
- Solitary cyst > 2.5 cm
- Solitary cyst of any size with thick walls, septations, papillary projections, calcifications and debris.
- Multiple hepatic calcifications or cluster > 01 cm.
- Multiple hepatic cysts of any size.
- Any haemangioma irrespective of the size and location.
- Portal vein thrombosis
- Evidence of portal hypertension (PV >13 mm, collaterals, ascites).
- Fit
General Instructions
GENERAL PHYSICAL ASSESSMENT
MEASUREMENTS AND PHYSIQUE
Appendix A
WEIGHT FOR HEIGHT CHART: MALES (AT ENTRY)
| Height in cm | Minimum Weigth in Kg | Maximum Weigth in Kg | ||
|---|---|---|---|---|
| Age at last birthday Below 20 yrs | Age at last birthday 20 to 25 yrs | Age at last birthday Above 25 yrs | ||
| 152 | 40 | 53 | 55 | 58 |
| 153 | 40 | 54 | 56 | 59 |
| 154 | 40 | 55 | 57 | 59 |
| 155 | 41 | 55 | 58 | 60 |
| 156 | 41 | 56 | 58 | 61 |
| 157 | 42 | 57 | 59 | 62 |
| 158 | 42 | 57 | 60 | 62 |
| 159 | 43 | 58 | 61 | 63 |
| 160 | 44 | 59 | 61 | 64 |
| 161 | 44 | 60 | 62 | 65 |
| 162 | 45 | 60 | 63 | 66 |
| 163 | 45 | 61 | 64 | 66 |
| 164 | 46 | 62 | 65 | 67 |
| 165 | 46 | 63 | 65 | 68 |
| 166 | 47 | 63 | 66 | 69 |
| 167 | 47 | 64 | 67 | 70 |
| 168 | 48 | 65 | 68 | 71 |
| 169 | 49 | 66 | 69 | 71 |
| 170 | 49 | 66 | 69 | 72 |
| 171 | 50 | 67 | 70 | 73 |
| 172 | 50 | 68 | 71 | 74 |
| 173 | 51 | 69 | 72 | 75 |
| 174 | 51 | 70 | 73 | 76 |
| 175 | 52 | 70 | 74 | 77 |
| 176 | 53 | 71 | 74 | 77 |
| 177 | 53 | 72 | 75 | 78 |
| 178 | 54 | 73 | 76 | 79 |
| 179 | 54 | 74 | 77 | 80 |
| 180 | 55 | 75 | 78 | 81 |
| 181 | 56 | 75 | 79 | 82 |
| 182 | 56 | 76 | 79 | 83 |
| 183 | 57 | 77 | 80 | 84 |
| 184 | 58 | 78 | 81 | 85 |
| 185 | 58 | 79 | 82 | 86 |
| 186 | 59 | 80 | 83 | 86 |
| 187 | 59 | 80 | 84 | 87 |
| 188 | 60 | 81 | 85 | 88 |
| 189 | 61 | 82 | 86 | 89 |
| 190 | 61 | 83 | 87 | 90 |
| 191 | 62 | 84 | 88 | 91 |
| 192 | 63 | 85 | 88 | 92 |
| 193 | 63 | 86 | 89 | 93 |
| 194 | 64 | 87 | 90 | 94 |
| 195 | 65 | 87 | 91 | 95 |
| 196 | 65 | 88 | 92 | 96 |
| 197 | 66 | 89 | 93 | 97 |
| 198 | 67 | 90 | 94 | 98 |
| 199 | 67 | 91 | 95 | 99 |
| 200 | 68 | 92 | 96 | 100 |
Appendix B
WEIGHT FOR HEIGHT CHART: FEMALES (AT ENTRY)
| Height in cm | Minimum Weigth in Kg | Maximum Weigth in Kg | ||
|---|---|---|---|---|
| Age at last birthday Below 20 yrs | Age at last birthday 20 to 25 yrs | Age at last birthday Above 25 yrs | ||
| 147 | 37 | 45 | 48 | 51 |
| 147 | 37 | 45 | 48 | 51 |
| 148 | 37 | 46 | 48 | 51 |
| 149 | 37 | 47 | 49 | 52 |
| 150 | 37 | 47 | 50 | 53 |
| 151 | 37 | 48 | 50 | 54 |
| 152 | 37 | 49 | 51 | 54 |
| 153 | 37 | 49 | 51 | 55 |
| 154 | 38 | 50 | 52 | 56 |
| 155 | 38 | 50 | 53 | 56 |
| 156 | 39 | 51 | 54 | 57 |
| 157 | 39 | 52 | 54 | 58 |
| 158 | 40 | 52 | 55 | 59 |
| 159 | 40 | 53 | 56 | 59 |
| 160 | 41 | 54 | 56 | 60 |
| 161 | 41 | 54 | 57 | 61 |
| 162 | 42 | 55 | 58 | 62 |
| 163 | 43 | 56 | 58 | 62 |
| 164 | 43 | 56 | 59 | 63 |
| 165 | 44 | 57 | 60 | 64 |
| 166 | 44 | 58 | 61 | 65 |
| 167 | 45 | 59 | 61 | 66 |
| 168 | 45 | 59 | 62 | 66 |
| 169 | 46 | 60 | 63 | 67 |
| 170 | 46 | 61 | 64 | 68 |
| 171 | 47 | 61 | 64 | 69 |
| 172 | 47 | 62 | 65 | 70 |
| 173 | 48 | 63 | 66 | 70 |
| 174 | 48 | 64 | 67 | 71 |
| 175 | 49 | 64 | 67 | 72 |
| 176 | 50 | 65 | 68 | 73 |
| 177 | 50 | 66 | 69 | 74 |
| 178 | 51 | 67 | 70 | 74 |
| 179 | 51 | 67 | 70 | 75 |
| 180 | 52 | 68 | 71 | 76 |
| 181 | 52 | 69 | 72 | 77 |
| 182 | 53 | 70 | 73 | 78 |
| 183 | 54 | 70 | 74 | 79 |
| 184 | 54 | 71 | 74 | 80 |
| 185 | 55 | 72 | 75 | 80 |
| 186 | 55 | 73 | 76 | 81 |
| 187 | 56 | 73 | 77 | 82 |
| 188 | 57 | 74 | 78 | 83 |
| 189 | 57 | 75 | 79 | 84 |
| 190 | 58 | 76 | 79 | 85 |
| 191 | 58 | 77 | 80 | 86 |
| 192 | 59 | 77 | 81 | 87 |
| 193 | 60 | 78 | 82 | 88 |
| 194 | 60 | 79 | 83 | 88 |
| 195 | 61 | 80 | 84 | 89 |
- Fit
- Normal echo-anatomy of the gall bladder.
- Post Laparoscopic Cholecystectomy. After eight weeks, provided LFT and histopathology are within normal limits.
- Post Open Cholecystectomy. After 24 weeks, provided LFT and histopathology are within normal limits and in the absence of incisional hernia as confirmed on USG Abdomen.
- Unfit
- Cholelithiasis or biliary sludge.
- Choledocolithiasis.
- Polyp of any size and number.
- Choledochal cyst.
- Gall bladder mass.
- Gall bladder wall thickness > 05 mm.
- Septate gall bladder.
- Persistently contracted gall bladder on repeat USG.
- Incomplete Cholecystectomy.
- Non-visualized Gall Bladder on USG Will be considered unfit. They will be considered fit during appeal, if agenesis of gall bladder is confirmed on Magnetic Resonance Cholangio-Pancreatography (MRCP), in the absence of any other abnormality of the biliary tract.
- Unfit
- Spleen more than 13 cm in longitudinal axis (or if clinically palpable).
- Any Space Occupying Lesion in the spleen.
- Asplenia.
- Candidates who have undergone partial/ total splenectomy are unfit, irrespective of the cause of operation.
- Unfit
- Any structural abnormality.
- Space Occupying Lesion/ Mass lesion.
- Features of chronic pancreatitis (calcification, ductal abnormality, atrophy).
- Unfit
- Ascites.
- Solitary mesenteric or retroperitoneal lymph node >1 cm. (Single retroperitoneal LN <1 cm and normal in architecture may be considered fit).
- Two or more lymph nodes of any size.
- Any mass or cyst.
- Laparoscopic Appendectomy will be assessed
for post-operative fitness after a minimum period of 04
weeks. Candidates will be considered fit if: -
- Post site scars have healed well
- Scars are supple
- Histo-pathological report of acute appendicitis is available.
- USG confirmation of absence od port site incisional hernia
- Open Appendectomy (appendicectomy through
right iliac fossa incision only) will be assessed for
post-op fitness after a minimum period 12 weeks.
Candidates will be considered fit if: -
- Wound has healed well
- Scar is supple and non tender
- Histo-pathological report of acute appendicitis is available
- USG confirmation of absence of surgical site incisional hernia
The fitness criteria to be followed are as follows:-
- Unfit
- If the testis cannot be palpated (unilateral or bilateral) even after examination of the candidate in squatting position.
- Bilateral orchidectomy due to any cause such as trauma, torsion or infection is unfit.
- Fit
- Operatively corrected UDT at least four weeks after surgery, provided after surgical correction, the testis is normal in location and the wound has healed well.
- Unilateral orchidectomy for benign cause, provided other testis is normal in size, fixation and location.
- Unfit – Bilateral atrophied testis.
- Fit - Unilateral atrophic testis for benign cause, provided other testis is normal in size, fixation and location. .
- Unfit – All grades of current varicocele.
- Fit - Post-operative cases of varicocele with no residual varicocele and no post-op complications or testicular atrophy after eight weeks of surgery.
- Unfit – Current hydrocele on any side.
- Fit - Operated cases of hydrocele after eight weeks of surgery, if there are no post-op complications and wound has healed well.
- Unfit – Current presence of cyst / mass.
- Fit – After 08 Weeks of Post-operative well healed cases with no recurrence and only when benign on histopathology report.
- Unfit – Presence of current orchitis or epididymitis/ tuberculosis.
- Fit – After treatment, provided the condition has resolved completely.
- Unfit – All are unfit, except glanular variety of hypospadias and epispadias, which is acceptable.
- Fit – Post-operative cases at least 08 weeks after successful surgery, provided recovery is complete and there are no complications.
- Unfit – Current phimosis, if tight enough to interfere with local hygiene and voiding and/ or associated with Balanitis Xerotica Obliterans.
- Fit – Operated cases will be considered fit after 04 weeks of surgery, provided wound is fully healed and no post-op complications are seen.
- Unfit – Current disease, if small enough to interfere with voiding.
- Fit – Mild disease not interfering with voiding and post-operative cases after a period of 04 weeks of surgery with adequately healed wound and no Post Operative complications.
- Proteinuria. . Proteinuria will be a cause for rejection, unless it proves to be orthostatic.
- Glycosuria. When glycosuria is detected, a blood sugar examination (fasting and after 75 g glucose) and glycosylated Hb is to be carried out, and fitness decided as per results. Renal glycosuria is not a cause for rejection.
- Urinary Infections. When the candidate has history or evidence of urinary infection it will entail full renal investigation. Persistent evidence of urinary infection will entail rejection.
- Haematuria. Candidates with history of haematuria will be subjected to full renal investigation.
- Acute. Acute: In this condition there is a high rate of recovery in the acute phase, particularly in childhood. A candidate who has made a complete recovery and has no proteinuria may be assessed fit, after a minimum period of one year after full recovery.
- Chronic. Candidate with chronic glomerulonephritis will be rejected.
- Unfit
- Congenital structural abnormalities of kidneys or
urinary tract
- Unilateral renal agenesis.
- Unilateral or bilateral hypoplastic/ contracted kidney of size less than 08 cm.
- Malrotation of kidney.
- Horseshoe kidney.
- Ptosed kidney.
- Crossed fused/ ectopic kidney.
- Simple single renal cyst of more than 1.5 cm size in one kidney.
- Complex cyst/ polycystic disease/ multiple or bilateral cysts.
- Renal/ ureteric/ vesical mass.
- Hydronephrosis or Hydroureteronephrosis.
- Calculi - Renal/ Ureteric/ Vesical.
- Calyectasis
- Congenital structural abnormalities of kidneys or
urinary tract
- Fit - Solitary, unilateral, simple renal cyst < 1.5 cm provided the cyst is peripherally located, round/ oval, with thin smooth wall and no loculations, with posterior enhancement, no debris, no septa and no solid component.
- There is a well healed surgical wound with no residual disease
- No post operative complication
- Surgical scar should be sufficiently matured and unlikely to cause any problems during military training
- Normal general physical examination
- Endocrine workup is normal
- If clinical examination reveals restriction of spine movements, deformities, tenderness of the spine or any gait abnormalities, it will be considered unfit.
- Gross kyphosis, affecting military bearing/ restricts full range of spinal movements and/or expansion of chest is unfit.
- When scoliosis is noticeable or any pathological condition of the spine is suspected, radiographic examination of the appropriate part of the spine needs to be carried out. Scoliosis is unfit, if deformity persists on full flexion of the spine, when associated with restricted range of spine movements or when due to an underlying pathological cause.
- Congenital defects overlying the spine e.g. hypertrichosis, skin dimpling, haemangioma, pigmented naevus or dermal sinus.
- Presence of lipoma over spine.
- Palpable spina bifida.
- Abnormal findings on neurological examination.
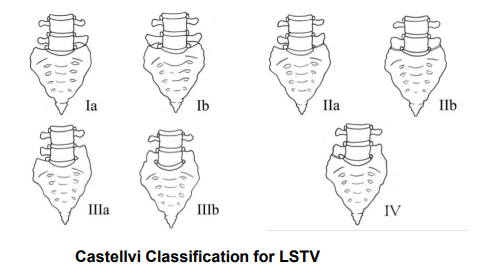
- Type I. Enlarged and dysplastic transverse process
(at least 19 mm in width in craniocaudal dimension).
- I a. Unilateral.
- I b. Bilateral.
- Type II. Pseudoarticulation of the transverse
process and sacrum with incomplete
lumbarisation/sacralistion (enlargement of the transverse
process with pseudoarthrosis).
- II a. Unilateral.
- II b. Bilateral.
- Type III. Transverse process fuses with the sacrum
and there is complete lumbarisation or sacralisation
(enlarged transverse process with complete fusion).
- III a. Unilateral.
- III b. Bilateral.
- Type IV. Type II on one side and type III on the contralateral side.
- Congenital/ Developmental Anomalies
- Wedge Vertebra.
- Hemivertebra
- Anterior Central Defect.
- Cervical Ribs (Unilateral/Bilateral) with demonstrable neurological or circulatory deficit.
- Spina Bifida. All types are unfit except in sacrum and LV5 (if completely sacralised).
- Loss of Cervical Lordosis with neurological deficit.
- Assessment of Scoliosis. Idiopathic scoliosis upto
10 degrees for Lumbar Spine and 15 degrees for Dorsal Spine
will be acceptable provided:-
- Individual is asymptomatic
- No history of trauma to spine
- No chest asymmetry/shoulder imbalance or pelvic obliquity in the lumbar spine.
- There is no neurological deficit
- No congenital anomaly of the spine
- There is absence of syndromic features
- ECG is normal
- No deformity exists on full flexion of the spine
- No restriction of range of movements
- No organic defect causing structural abnormality
- Atlanto-occipital and Atlanto-axial anomalies.
- Incomplete block vertebra at any level.
- Complete block vertebra at more than one level. (Single level is acceptable. Annotation is to be made in AFMSF-2).
- Lumbosacral Transitional Vertebra (LSTV). Unilateral sacralisation or lumbarisation (complete or incomplete) and Bilateral incomplete sacralisation or lumbarisation (LSTV- Castellvi Type II a and b, III a and IV). Bilateral Complete Sacralisation of LV5 and Bilateral Complete Lumbarisation of SV1, LSTV Castellvi Type III b, Type I a and b are acceptable (Annotation is to be made in AFMSF-2).
- Spondylolysis/Spondylolisthesis.
- Intervertebral Disc Prolapse.
- Schmorl ’s Nodes at more than one level.
- Traumatic Conditions
- Spondylolysis/ Spondylolisthesis
- Compression fracture of vertebra
- Intervertebral Disc Prolapse
- Schmorl’s Nodes at more than one level
- Infective
- Tuberculosis and other Granulomatous disease of spine (old or active)
- Infective Spondylitis
- Autoimmune
- Rheumatoid Arthritis and allied disorders
- Ankylosing spondylitis
- Other rheumatological disorders of spine e.g Polymyositis, SLE and Vasculitis
- Degenerative
- Spondylosis
- Degenerative Joint Disorders
- Degenerative Disc Disease
- Osteoarthrosis/ osteoarthritis
- Scheuerman’s Disease (Adolescent Kyphosis)
- Any other spinal abnormality, if so considered by the specialist.
- Polydactyly Can be assessed for fitness 12 weeks post op. Can be declared fit if there is no bony abnormality(X-Ray), wound is well healed, scar is supple and there is no evidence of neuroma on clinical examination.
- Simple syndactyly Can be assessed for fitness 12 weeks post op. Can be declared fit if there is no bony abnormality(X-Ray), wound is healed, scar is supple and webspace is satisfactory.
- Complex syndactylyUnfit
- Hyperextensible finger joints All candidates shall be thoroughly examined for hyperextensible finger joints. Any extension of fingers bending backwards beyond 90 degrees shall be considered hyper extensible and considered unfit. Other joints like knee, elbow, spine and thumb shall also be examined carefully for features of hyper laxity/hypermobility. Although the individual may not show features of hyper laxity in other joints, isolated presentation of hyper extensibility of finger joints shall be considered unfit because of the various ailments that may manifest later if such candidates are subjected to strenuous physical training.
- Mallet Finger Loss of extensor mechanism at the distal interphalangeal joint leads to Mallet finger. Chronic mallet deformity can lead to secondary changes in the PIP and MCP joint which can result in compromised hand function. Normal range of movement at DIP joints is 0-80 degree & PIP joint is 0-90 degrees in both flexion and extension. In Mallet finger candidate is unable to extend/straighten distal phalanx of fingers completely.
- Candidates with mild condition i.e less than 10 degrees of extension lag without any evidence of trauma, pressure symptoms and any functional deficit should be declared Fit.
- Candidates with fixed deformity of fingers will be declared unfit.
- Measurement modality: Measured using a goniometer
- Recommendation: Normal elbow extension is 0 degrees. Up to 10 degrees of hyperextension is within normal limits if the patient has no history of trauma to the joint. Anyone with hyperextension more than 10 degrees should be unfit.
- If the arches of the feet reappear on standing on toes, if the candidate can skip and run well on the toes and if the feet are supple, mobile and painless, the candidate is acceptable.
- Rigid or fixed flat feet, gross flat feet, with planovalgus, eversion of heel, cannot balance himself on toes, cannot skip on the forefoot, tender painful tarsal joints, prominent head of talus will be considered unfit. Restriction of the movements of the foot will also be a cause for rejection. Rigidity of the foot, whatever may be the shape of the foot, is a cause for rejection.
- All intra-articular fractures especially of major joints (Shoulder, elbow, wrist, hip, knee and ankle) with or without surgery, with or without implant shall be considered unfit.
- All extra-articular fractures with post operative implant in-situ shall be considered unfit and will be considered for fitness after minimum of 12 weeks of implant removal.
- Nine (09) months will be the minimum duration for
considering evaluation following extra-articular injuries of
all long bones (both upper and lower limbs) post injury
which have been managed conservatively. Individual will be
considered fit if there is:-
- No evidence of mal alignment/malunion
- No neuro vascular deficit
- No soft tissue loss
- No function deficit
- No evidence of osteomyelitis/sequestra formation
- External Deformity of Nose or Deviated
Nasal Septum.
- Unfit - Gross external deformity of nose causing cosmetic deformity or obstruction to free breathing as a result of a marked septal deviation.
- On appeal - Post corrective surgery with residual mild deviation with adequate airway patency will be acceptable after four weeks post surgery.
- Septal Perforation- Unfit
- On appeal - Any anterior septal perforation/posterior septal perforation > 01 cm in the greatest dimension is a ground for rejection. A septal perforation which is associated with nasal deformity, nasal crusting, epistaxis and granulation irrespective of the size is a ground for rejection.
- On appeal - Post corrective surgery with residual mild deviation with adequate airway patency will be acceptable after four weeks post surgery.
- Atrophic rhinitis- Unfit.
- Any history/clinical evidence suggestive of allergic rhinitis/vasomotor rhinitis are to be declared Unfit
- Any infection of the para-nasal sinuses is to be declared Unfit. Such cases may be accepted following successful treatment at the Appeal Medical Board.
- Nasal polyposis. Unfit (treated or untreated).
- Unfit
- Current/ operated cases of leukoplakia, erythroplakia, submucous fibrosis, ankyloglossia and oral carcinoma.
- Current oral ulcers/ growths and mucous retention cysts.
- Trismus due to any cause.
- Cleft palate, even after surgical correction.
- Fit
- Completely healed oral ulcers after four weeks post-surgery with proven benign histopathology.
- Operated cases of mucus retention cyst with no recurrence and proven benign histology. Evaluation in these cases must be done after minimum four weeks postsurgery.
- Sub-mucous cleft of palate with or without bifid uvula not causing Eustachian tube dysfunction may be accepted by ENT specialist, provided PTA, tympanometry and speech are normal.
- Any ulcerative/ mass lesion of the pharynx.
- Candidates in whom tonsillectomy is indicated. Such candidates may be accepted minimum four weeks after successful surgery provided there are no sequelae and histology is benign.
- Cleft palate.
- Any disabling condition of the pharynx or larynx causing persistent hoarseness or dysphonia.
- Chronic laryngitis, vocal cord palsy, laryngeal polyps and growths.
- Hearing acuity below 600 cm in CV or FW.
- The audiometric loss greater than 20 db, in frequencies between 250 and 8000 Hz on PTA.
- Gross deformity of pinna which may hamper wearing of uniform/personal kit/ protective equipment, or which adversely impacts military bearing.
- Cases of chronic otitis externa.
- Any condition (ear wax, atresia/narrowing of external auditory meatus or neoplasm, exaggerated tortuosity of the canal, bony growth of external auditory canal) preventing a proper visualization of the tympanic membrane.
- Granulation or polyp in external auditory canal.
- Otitis Media: Current Otitis Media of any type will entail rejection. If evidence of healed chronic otitis media (in the form of tympanosclerosis/scarred tympanic membrane affecting only pars tensa part of tympanic membrane) and all operated cases of tympanoplasty/Myringotomy will be assessed by ENT specialist. They will be acceptable if Pure Tone Audiometry (PTA) and Tympanometry are normal. On appeal, a trial of decompression chamber may be carried out, if indicated, for aircrew, ATC/FC, submariners/divers.
- Any type of TM perforation or healed perforation/retraction in pars flaccida of the tympanic membrane is unfit.
- Marked retraction or restriction in TM mobility on pneumatic otoscopy.
- Tympanometry showing patterns other than Type ‘A’ tympanogram.
- Any implanted hearing devices eg, cochlear implants, bone-anchored hearing aids etc.
- After middle ear surgeries viz, stapedectomy, ossiculoplasty, any type of mastoidectomy.
- Otosclerosis.
- Meniere‘s disease.
- Vestibular dysfunction including nystagmus of vestibular origin.
- Bell‘s palsy following ear infection.
- Candidates, who are wearing spectacles or found to have defective vision, should be properly assessed. All cases of squint are unfit.
- Ptosis
- Candidates, who meet the following criteria are
Fit.
- Mild ptosis
- Clear visual axis
- Normal visual field
- No sign of aberrant degeneration/ head tilt
- Rest all cases - Unfit
- On appeal - Candidates who have undergone surgical correction may be considered fit provided one year has elapsed post-surgery with no recurrence, the abovementioned criteria are met and upper eyelid is not more than 02 mm below the superior limbus.
- Candidates, who meet the following criteria are
Fit.
- Exotropia Unfit
- Anisocoria If size difference between the pupils is >01 mm, candidate will be considered unfit.
- Heterochromia irides: Unfit
- Sphincter tears: Can be considered fit is size difference between pupils is <01 mm, pupillary reflexes are brisk with no observed pathology in cornea, lens or retina.
- Pseudophakia: Unfit
- Blepharitis Candidates with blepharitis, particularly with loss of eyelashes, must be rejected.
- Ectropion/Entropion. These cases are to be made unfit. On appeal, mild ectropion and entropion which in the opinion of ophthalmologist will not hamper day to day functioning in any way, may be made fit.
- Pterygium. All cases of pterygium are to be made unfit. On appeal, regressive nonvascularised pterygium occupying ≤ 1.5 mm of the peripheral cornea may be made fit by Eye Specialist after measurement on a slit lamp.
- Nystagmus. All cases of nystagmus are to be made unfit except for physiological nystagmus.
- Naso-lacrymal duct occlusion producing epiphora or a mucocele entails rejection.
- Active Uveitis (iritis, cyclitis and choroiditis) will be grounds for rejection. Candidates giving a history of this condition should be made unfit.
- Cornea.
- Unfit
- Corneal scars/opacities
- Any candidate with progressive corneal disorders viz, Corneal dystrophies, Keratoconus, Keratoglobus, any corneal degenerations.
- Any active corneal disorder
- On appeal corneal scars are acceptable if it does not interfere with vision.
- Unfit
- Lenticular opacities: Unfit
On appeal- Unfit- Any lenticular opacity that is causing visual deterioration or is in the visual axis or central area of 04 mm around the pupils is unfit. The propensity of the opacities not to increase in size or number should also be a considered.
- Fit - Small stationary lenticular opacities in the periphery like congenital blue dot cataract, not affecting the visual axis/visual field (should be less than 10 in number and central area of 04 mm should be clear).
- Optic Nerve Drusen Unfit
- High Cup- Disc ratio: Unfit, if any of
the following conditions exist:-
- Inter –Eye asymmetry in cup Disc ratio > 0.2
- Retinal Nerve fibre Layer (RNFL) defect seen by RNFL analysis on Optical Coherence Tomography (OCT).
- Visual Field defect detected by visual Field Analyser
- Migraine with visual symptoms are not a strictly ocular problem and should be assessed in accordance with para 124.
- As tests for night blindness are not routinely performed, a certificate to the effect that the individual does not suffer from night blindness will be obtained in every case. Certificate should be as per Appendix C to this chapter. A proven case of night-blindness is unfit.
- Restriction of movements of the eyeball in any direction and undue depression/prominence of the eyeball are unfit.
- Retinal lesions. A small healed chorio-retinal scar in the retinal periphery not affecting the vision and not associated with any other complications will be considered fit. Similarly, a small lattice in periphery with no other complications will be made fit. Any lesion in the central fundus will be made unfit.
- Lattice degeneration.
- The following lattice degeneration will render a
candidate unfit:-
- Single circumferential lattice extending more than two clock hours in either or both eyes.
- Two circumferential lattices, each more than one clock hour in extent in either or both eyes.
- Radial lattices.
- Any lattice with atrophic hole/flap tears (Unlasered).
- Lattice degeneration posterior to equator.
- Candidates with lattice degeneration will be
considered fit under the following conditions: -
- Single circumferential lattice without holes of less than two clock hours in either or both eyes.
- Two circumferential lattices without holes each being less than one clock hour in extent in either or both eyes.
- Post-laser delimitation, single circumferential lattice, without holes/flap tear, less than two clock hours extent in either or both eyes.
- Post-laser delimitation, two circumferential lattices, without holes/flap tear, each being less than one clock hour extent in either or both eyes.
- The following lattice degeneration will render a
candidate unfit:-
- Keratoconus: Keratoconus is Unfit.
- Unfit, if outside the prescribed visual limits.
- Unfit even if the corrected visual acuity is within
the acceptable limits when:-
- There is a strong family history of high myopia, and that the visual defect is recent onset.
- If physical growth is still expected.
- If the fundus appearance is suggestive of progressive myopia.
- Fit
- Candidates for IAF meeting the visual requirements for the branch as laid down in Appendix D to para 146. Residual refraction after such procedure should not be more than +/- 1.0 D Sph or Cyl for branches where correctable refractive errors are permitted.
- Keratorefractive Surgery must not have been carried out before the age of 20 years.
- At least 12 months must have elapsed post uncomplicated stable Keratorefractive Surgery with no history or evidence of any complication.
- The axial length of the eye must not be more than 26 mm as measured by IOL master.
- The post Keratorefractive Surgery corneal thickness as measured by a corneal Pachymeter must not be less than 450 microns.
- Unfit
- Radial Keratotomy (RK) surgery for correction of refractive errors
- Individuals with high refractive errors (> 6 D) prior to Keratorefractive Surgery.
- Convergence (as assessed on RAF rule)
- Objective Convergence.
- Up to 10 cm- Fit.
- More than 10 cm - Unfit.
- Subjective Convergence (SC). . This indicates the end point of binocular vision under the stress of convergence. If the subjective convergence is more than 10 cm beyond the limit of objective convergence, the fusion capacity is poor. This is specially so when the objective convergence is 10 cm and above.
- Objective Convergence.
- Accommodation. In the case of myopes,
accommodation should be assessed with corrective glasses in
position. The acceptable values for accommodation in various
age groups are given in Table 1.
Table 1 -Accommodation Values – Age wise
Age in Yrs 17-20 21-25 26-30 31-35 36-40 41-45 Accommodation (in cm) 10-11 11-12 12.5-13.5 14-16 16-18.5 18.5-27
Appendix C
Certificate Regarding Night Blindness
Name with Initials
__________________________________________________ Batch No.
_____________________ Chest No __________________________
I hereby certify that to the best of my knowledge, there has not been any case of night blindness in our family, and I do not suffer from it.
Date: ………………………………. (Signature of the candidate)
I hereby certify that to the best of my knowledge, there has not been any case of night blindness in our family, and I do not suffer from it.
Date: ………………………………. (Signature of the candidate)
Countersigned by
(Name of Medical Officer)
Appendix D
VISUAL STANDARDS FOR OFFICERS, CADETS AND AIRMEN AIRCREW AT INITIAL ENTRY
| SL No | Med Cat | Branch | Maximum Limits of Refractive Error | Visual Acuity ErrorsVisual Acuity (VA) with Limits of Maximum Correction | Colour Vision |
| 1 | A1G1 | F(P) including WSOs/CSOs, Flying Branch Cadets at NDA and AFA | Hypermetropia: +1.5 D Sph Manifest Myopia: Nil Astigmatism: + 0.75 D Cyl (within +1.5 D Max) Retinoscopic Myopia: Nil |
6/6 in one eye and 6/9 in other, correctable to 6/6 both eyes only for Hypermetropia | CP-I |
| 2 | A4G1 | Aircrew other than F(P) | Hypermetropia: +3.5 D Sph Myopia: -2.0 D Sph Astigmatism: ± 0.75 D Cyl |
6/24 in one eye and 6/36 in other, correctable to 6/6 both eyes | CP-I |
| 3 | A4G1 | Adm/ATC/FC/ WS | Hypermetropia: +3.5 D Sph Myopia: -3.50 D Sph Astigmatism: ±2.50 D Cyl |
Correctable to 6/6 in each eye. Wearing of glasses will be compulsory when visual acuity is below 6/6 | CP-II |
| 4 | A4G1 | AE(M)/ AE(L) | Hypermetropia: +3.5 D Sph Myopia: -3.50 D Sph Astigmatism: ±2.50 D Cyl |
Corrected visual acuity must be 6/6 in each eye. Wearing of glasses will be compulsory when advised. | CP-II |
| 5 | A4G1 | Met | Hypermetropia: +3.5 D Sph Myopia: -3.50 D Sph Astigmatism: ±2.50 D Cyl |
Corrected visual acuity must be 6/6 both eyes. Wearing of glasses will be compulsory. | CP-II |
| 6 | A4G1 | Accts/ Lgs/Edn | Hypermetropia: +3.5 D Sph Myopia: -3.50 D Sph Astigmatism: ±2.50 D Cyl |
Corrected visual acuity must be 6/6 both eyes. Wearing of glasses will be compulsory. | CP-II |
| 8 | A4G1 | 10+2/NDA Entry to ground Duty Branches of IAF (AE(L)/ADM/LGS) | Hypermetropia: +2.5 D Sph Myopia: -2.50 D Sph Astigmatism: ±2.0 D Cyl |
Uncorrected VA 6/36 and 6/36 Corrected VA 6/6 and 6/6 | CP-II |
Notes:
Note1. Ocular muscle balance for personnel covered in Ser No. 1 and 2 must conform to Appendix C to this Chapter.Note2. Visual standards of Air Wing Cadets at NDA and Flt Cdts of F(P) at AFA must conform to A1G1 F(P) standard (Ser No. 1 of Appendix B).
Note3. The Sph correction factors mentioned above will be inclusive of the specified astigmatic correction factor. A minimum correction factor upto the specified visual acuity standard can be accepted.
Note4. Medical Standards of Medical and Dental Officers are as notified by o/o DGAFMS, as amended from time to time.
Appendix E
Standard of Ocular Muscle Balance for Flying Duties
| Sl No | Test | Fit |
| 1 | Maddox Rod Test at 6 meters | Exo- 06 Prism D Eso- 06 Prism D Hyper- 01 Prism D Hypo- 01 Prism D |
| 2 | Maddox Rod Test at 33 cm | Exo-16 Prism D Eso- 06 Prism D Hyper- 01 Prism D Hypo- 01 Prism D |
| 3 | TNO Test or Titmus Fly Test | All of BSV grades |
| 4 | Convergence | Up to 10 cm |
| 5 | Cover Test for Distance and Near | Latent divergence /convergence recovery rapid and complete |
- All cases of anemia (<13 g/dL in males and <12 g/dL in females) will be declared unfit during SMB.
- All candidates with evidence of hereditary haemolytic anaemias (due to red cell membrane defect or due to red cell enzyme deficiencies) and haemoglobinopathies (Sickle cell disease, BetaThalassaemia: Major, Intermedia, Minor, Trait and Alpha Thalassaemia etc) are to be considered unfit for service.
- Candidates with history of haemophilia or von Willebrand’s disease are to be declared unfit. Candidates with clinical evidence of purpura or evidence of thrombocytopenia are to be considered unfit. Cases of Purpura Simplex (simple easy bruising), a benign disorder seen in otherwise healthy women, may be accepted.
- Monocytosis. Absolute monocyte counts greater than 1000/cumm or more than or equal to 10% of total WBC is to be deemed unfit.
- Eosinophilia. Absolute eosinophil counts greater than or equal to 500/cumm is deemed unfit.
- Haemoglobin more than 16.5 g/dL in males and more than 16 g/dL in females will be considered as Polycythemia and deemed Unfit.
- Dental Standards.
- Candidate must have a total minimum of 14 dental
points and the following teeth must be present in the upper
jaw in good functional opposition with the corresponding
teeth in the lower jaw.
- Any four of the six anterior.
- Any six of the ten posterior.
- The above dental standards are to be followed and candidates who do not conform to the laid down standards will be rejected.
- Candidate must have a total minimum of 14 dental
points and the following teeth must be present in the upper
jaw in good functional opposition with the corresponding
teeth in the lower jaw.
- Extra Oral Examination.
- Gross Facial Examination. Presence of any gross asymmetry or soft/hard tissue defects/scars or if any incipient pathological condition of the jaw is suspected, it will be a cause of rejection.
- Functional Examination.
- Temporo-Mandibular Joint (TMJ). TMJs will be bilaterally palpated for tenderness and/or clicking. Candidates with symptomatic clicking and/or tenderness or dislocation of the TMJ on wide opening will be rejected.
- Mouth Opening. A mouth opening of less than 30 mm measured at the incisal edges will be reason for rejection.
- Guidelines for Awarding Dental Points
in Special Situations.
- Dental caries. Teeth with caries that have not been restored or teeth associated with broken down crowns, pulp exposure, residual root stumps, teeth with abscesses and/or sinuses will not be counted for award of dental points.
- Restorations. Teeth having restorations that appear to be improper/broken/discolored will not be awarded dental points. Teeth restored by use of inappropriate materials, temporary or fractured restorations with doubtful marginal integrity or peri-apical pathology will not be awarded dental points.
- Loose Teeth. Loose/mobile teeth with clinically demonstrable mobility will not be awarded dental points. Periodontally splinted teeth will not be counted for award of dental points.
- Retained Deciduous Teeth. Retained deciduous teeth will not be awarded dental points.
- Morphological Defects. Teeth with structural defects which compromise efficient mastication will not be awarded dental points.
- Periodontium.
- The condition of the gums, of the teeth included for counting dental points, should be healthy ie pink in colour, firm in consistency and firmly resting against the necks of the teeth. Visible calculus should not be present.
- Individual teeth with localized periodontitis (swollen, red or infected gums or those with visible calculus) will not be awarded dental points.
- Candidates with severe periodontal disease (generalized calculus, extensive swollen and red gums, with or without exudates), shall be rejected. If periodontal disease is not severe and the teeth are otherwise sound, the candidate may be accepted if in the opinion of the Dental Officer, he/she can be cured by simple periodontal therapy excluding extraction.
- Malocclusion. Candidates with
malocclusion affecting masticatory efficiency and phonetics
shall not be selected. Teeth in open bite will not be
awarded dental points as they are not considered to be in
functional apposition. Candidates having an open bite,
reverse overjet or any visible malocclusion will be
rejected. However, if in the opinion of the Dental Officer,
the malocclusion of teeth is not hampering efficient
mastication, phonetics, maintenance of oral hygiene or
general nutrition or performance of duties efficiently,
then candidates will be declared fit. The following
criteria have to be considered in assessing malocclusion:-
- Edge to Edge Bite. Edge to edge bite will be considered as functional apposition.
- Anterior Open Bite. Anterior open bite is to be taken as lack of functional opposition of involved teeth.
- Cross Bite. Teeth in cross bite may still be in functional occlusion and may be awarded points, if so.
- Traumatic Bite. Anterior teeth involved in a deep impinging bite which is causing traumatic indentations on the palate will not be counted for award of points.
- Hard and Soft tissues. Soft tissues of cheek, lips, palate, tongue and sublingual region and maxilla/mandibular bony apparatus must be examined for any swelling, discoloration, ulcers, scars, white patches, sub mucous fibrosis etc. All potentially malignant lesions will be cause for rejection. Clinical diagnosis for sub-mucous fibrosis with or without restriction of mouth opening will be a cause of rejection. Bony lesion(s) will be assessed for their pathological/physiological nature and commented upon accordingly. Any hard or soft tissue lesion will be a cause of rejection.
- Orthodontic Appliances. Fixed orthodontics lingual retainers will not be considered as periodontal splints and teeth included in these retainers will be awarded points for dental fitness. Candidates wearing fixed or removable orthodontic appliances will be declared unfit.
- Dental Implants. Implants and Implant Supported Prosthesis will not be awarded any dental points. In the case of ex-serviceman applying for re-enrolment, dental points will be awarded for removal dental prosthesis.
- Fixed Partial Dentures (FPD)/Implant supported FPDs. FPDs will be assessed clinically and radiologically for firmness, functional apposition to opposing teeth and periodontal health of the abutments. If all parameters are found satisfactory, dental points will be awarded for the natural tooth (abutments). Note:- Any prosthesis, removable/fixed or implant borne, the natural tooth/teeth in that component will be awarded dental points.
- The Following will be Criteria for
Declaring a Candidate Unfit:-
- Oral Hygiene. Poor oral health status in the form of gross visible calculus, periodontal pockets and/or bleeding from gums will render candidate unfit.
- Candidates Reporting Post Maxillo-Facial Surgery/Maxillofacial Trauma. Candidates who undergo cosmetic or post-traumatic maxillofacial surgery/trauma will be UNFIT for at least 24 weeks from the date of surgery/injury whichever is later. After this period, if there is no residual deformity or functional deficit, they will be assessed as per the laid down criteria.
- Candidate with dental arches affected by advanced stage of generalized active lesions of pyorrhoea, acute ulcerative gingivitis, and gross abnormality of the teeth or jaws or with numerous caries or septic teeth will be rejected.
- History. Detailed menstrual and obstetric history, in addition to general medical history, must be taken and recorded. If a history of menstrual, obstetric or pelvic abnormality is given, an opinion of gynaecologist is to be obtained.
- General Medical and Surgical Standards
- Any lump in the breast will be a cause for rejection. Cases of fibroadenoma breast after successful surgical removal may be considered fit with the opinion of a surgical specialist and a normal histopathological report.
- Galactorrhoea will be cause for unfitness. Fitness after investigation/ treatment may be considered based on merits of the case and opinion of the concerned specialist during AMB.
- Amazia, Polymazia and Polythelia (Accessory nipple) will be considered unfit during SMB. Operated cases of Polymazia/Polythelia will be considered fit after 12 weeks of post-operative period after excision, if there is a well healed surgical wound and no post-operative complications.
- Gynaecological Examination. Any
abnormality of external genitalia will be considered on
merits of each case.
- Following conditions are acceptable:-
- Congenital elongation of cervix which comes up to introitus.
- Arcuate type of congenital uterine anomaly.
- Following conditions will entail rejection:-
- Amenorrhoea will be grounds for rejection. Such candidates will be investigated, and fitness will be considered on merits after examination and investigations during AMB.
- Severe menorrhagia or/and severe dysmenorrhoea.
- Stress urinary incontinence.
- (iv) Congenital elongation of cervix or complete prolapse which comes outside the introitus even after corrective surgery. (Complete prolapse of uterus will be a cause for rejection. Minor degree, after surgical correction, may be considered for fitness on merits.)
- Acute or chronic pelvic infection, Endometriosis and Adenomyosis.
- Disorders of sexual differentiation.
- Significant hir sutism especially with male pattern of hair growth.
- Any other gynaecological condition not covered above will be considered on merits of each case by Gynecologist.
- Following conditions are acceptable:-
- Current pregnancy would be a cause for rejection. The
minimum period after which the candidate will be reviewed for
appeal post pregnancy would be as follows: -
- Vaginal delivery. 24 weeks after an uncomplicated vaginal delivery.
- MTP/Abortion. Minimum four weeks and up to 12 weeks.
- Caesarean section. 52 weeks after uncomplicated caesarean section delivery.
- The individual would then be examined by the Gynaecologist and assessed regarding her fitness. In cases wherein more than six months have elapsed, after the initial medical examination, the candidate would be subjected to repeat complete medical examination as per the existing regulations.
- Ultrasonography of Lower Abdomen and Pelvis for Women
Candidates. This would be done as per existing orders: -
- Fit.
- Single small fibroid uterus (03 cm or less in diameter) without symptoms.
- Unilocular clear ovarian cyst less than 06 cm in diameter.
- Congenital elongation of cervix (which comes up to introitus).
- Arcuate uterus type of congenital uterine anomaly.
- Minimal fluid in Pouch of Douglas.
- Unfit.
- Candidates with fluid in Pouch of Douglas with internal echoes.
- Uterus. Absence of uterus or any congenital structural abnormality, except Arcuate uterus.
- Fibroids.
- Multiple fibroids more than two in number, with larger one > 15 mm in size.
- Single fibroid larger than 03 cm in size.
- Any fibroid causing distortion of endometrial cavity.
- Adenomyosis.
- Adnexa.
- Simple ovarian cyst 06 cm or more in size.
- Complex ovarian cyst of any size.
- Endometriosis.
- Hydrosalpinx.
- During Appeal Medical Board/Review Medical Board,
unfit candidates will be subjected to specific
investigations and detailed clinical examination. Fitness
for specific conditions will be decided as given below: -
- Fluid in POD with internal echoes will be assessed with TLC, DLC and C-Reactive Protein. Senior Adviser (Obs and Gynae) to opine on fitness.
- Endometrial thickness > 15 mm or residual echogenic shadows in endometrial cavity. Senior Adviser (Obs and Gynae) to opine on fitness.
- Fit.
- Medical Fitness after Laparoscopic Surgery or Laparotomy. Candidates reporting after undergoing cystectomy or myomectomy will be accepted as fit, if the candidate is asymptomatic, ultrasound pelvis is normal, histopathology report of removed tissue shows benign pathology and per operative findings are not suggestive of endometriosis. Fitness to be considered after laparoscopic surgery once the wound has healed fully. Candidate will be considered FIT after caesarean section and laparotomy after one year of the surgical procedure.
SELF CERTIFICATION CERTIFICATE (ONE FOR EACH TATTOO) BY CANDIDATES FROM TRIBAL COMMUNITIES WITH PERMANENT BODY TATTOO(S)
1. I, __________________________________________________ (Name
of Candidate). Son/Daughter of _____________________ (Name of
Father/Mother/Guardian as applicable)
__________________________(Date of Birth) hereby give an
undertaking that I belong to ______________ Tribe from
____________ area of _______________ state and * I do not have
any permanent body tattoo on my body/* I have _____ no of
permanent body tattoo (s) inked on my body as follows (one for
each tattoo) (*strike out whichever is not applicable):-
2. I am enclosing Certificate (s) as per Appendix B, in original, for permanent body tattoo(s) on my body, duly signed as per instructions.
3. I hereby declare that besides the tattoo(s) as referred in Para 1 of Appendix A above, I will not have any other permanent body tattoo(s) in future if I am selected to undergo pre-commissioning training.
4. The above information given by me is true and correct to the best of my knowledge and belief.
5. I understand and is aware that misrepresentation of any facts/concealment of any information
regarding permanent body tattoo(s) will lead to cancellation of my candidature at any stage from commencement of the selection process for which I shall be solely responsible.
| Photograph of Tattoo | Details of Tattoo |
| (Post card size to be pasted here duly signed by the candidate with name. Please do not use staple pins/clips | Size of Tattoo (in Cms) Language (if Applicable) Significance of Tattoo (if Applicable) |
2. I am enclosing Certificate (s) as per Appendix B, in original, for permanent body tattoo(s) on my body, duly signed as per instructions.
3. I hereby declare that besides the tattoo(s) as referred in Para 1 of Appendix A above, I will not have any other permanent body tattoo(s) in future if I am selected to undergo pre-commissioning training.
4. The above information given by me is true and correct to the best of my knowledge and belief.
5. I understand and is aware that misrepresentation of any facts/concealment of any information
regarding permanent body tattoo(s) will lead to cancellation of my candidature at any stage from commencement of the selection process for which I shall be solely responsible.
Place:
Date:……………………………….
Date:……………………………….
(Signature of the candidate)
Name, Entry & AFSB Batch No
Name, Entry & AFSB Batch No
Appendix F
CERTIFICATE (ONE CERTIFICATE FOR EACH TATTOO) FOR PERMANENT BODY TATTOO IN RESPECT OF CANDIDATES FROM TRIBAL COMMUNITIES
1. This is to certify that
________________________________________________ (Name of
Candidate) whose date of birth is _____________________ the
son/daughter of
________________________________________________ (Name of
Father/Mother/Guardian as applicable) and belongs to
______________________ (Name of the Tribe) Community of
____________________ (Name of the District) in the state of
________________________________________________ (Name of the
State).
2. It is certified that the permanent body tattoo(s) inked on the following parts of the body of ________________________________________________ (Name of Candidate) is/are as per existing customs and traditions of _____________________ Tribe and is prevalent as on date:-
Note- Separate photograph of each tattoo with details and description will be separately furnished and each page will be duly attested by the Authority.
2. It is certified that the permanent body tattoo(s) inked on the following parts of the body of ________________________________________________ (Name of Candidate) is/are as per existing customs and traditions of _____________________ Tribe and is prevalent as on date:-
| Photograph of Tattoo | Details of Tattoo |
| Post card size to be pasted here duly signed by the candidate and official issuing this certificate with respective names. Please do not use staple pins/clips | Size of Tattoo (in Cms) Language (if Applicable) Significance of Tattoo (if Applicable) |
Note- Separate photograph of each tattoo with details and description will be separately furnished and each page will be duly attested by the Authority.
Place:
Date:……………………………
Date:……………………………
Affix
round stamp
(Signature with Name, Designation and Stamp of DC/DM of
SDM of the District/Tehsil)OR
(Signature with Name, Designation if any and Address of
Chairman/Secretary of Senior Member of the Tribe to
which the candidate belongs to with their Stamp).
SDM of the District/Tehsil)OR
(Signature with Name, Designation if any and Address of
Chairman/Secretary of Senior Member of the Tribe to
which the candidate belongs to with their Stamp).
